You’ve decided that right now is not a good time to become pregnant. I’d wager that you’d like to pull this off without total abstinence! So, what are your options if you want to have sex and not have babies?
Obviously, there’s a number of different family planning options to choose from. You’re probably going to want to weigh the pros and cons of many different methods. Choosing a family planning method is a big decision—and there are a lot of factors to weigh as you decide which method is the best fit for you. A simple question probably tops your list: Does the method work? Will it help you to avoid pregnancy, or will you be surprised by a very cute baby? Can you trust the NFP statistics you find online?
No matter which method of family planning you choose, the answer to “Does the method work” is not a simple yes or no. If you’re having sex and want to avoid pregnancy there is an element of chance involved. No method of pregnancy avoidance is 100% effective, 100% of the time—except abstinence. It’s even possible (though highly unlikely) for men to father a child after having had a vasectomy (Schwingl & Guess, 2000). No method of family planning is 100% effective, but there are methods that are more effective than others. It may lead you to wonder… How does an “effective” method of pregnancy avoidance still result in pregnancy?
Today I’m going to give a little lesson in how medical research measures effectiveness rates. Think of this as a primer in natural family planning statistics.
I’m going to make the case, in plain language and using a silly example to illustrate, for the importance of considering and comparing both the perfect use effectiveness rate and the typical use effectiveness rate for any health care intervention you’re considering—whether that’s a contraceptive option, a natural family planning method like the Marquette Method of NFP, or something as simple as choosing the most effective pain medication.
Doctors decide which treatments to prescribe by evaluating effectiveness research—this is part of what “evidence-based medicine” means (Singal, 2014). NFP is heath care (reproductive health care, to be exact), and the Marquette Method’s protocols have been evaluated extensively in a number of peer-reviewed, published effectiveness studies.
Table of Contents
Perfect and Typical Use Effectiveness Rates
(and Why You Should Care)
In medical research, effectiveness rates come in pairs. Effectiveness studies report a perfect use effectiveness rate (also called the correct use effectiveness rate) and a typical use effectiveness rate. Both numbers are important, and they are meant to be compared to each other.
Effectiveness studies are a specific form of medical trial that’s aimed at determining how effective a treatment is in real-world conditions. Researchers enroll the study participants, teach them the instructions to use the treatment, and follow the progress of the participants over a specified period of time (in an effectiveness study for a family planning method, the study is generally one year long). At the end of the study, researchers evaluate who achieved the treatment’s desired outcome, and who didn’t. Then they crunch the numbers in two different ways:
The Perfect Use Effectiveness Rate
The perfect use effectiveness rate represents the percentage of people who followed the treatment instructions perfectly (e.g. they took their pill every day) and experienced the desired outcome (e.g. their disease was cured). Anyone who didn’t follow the treatment instructions perfectly is excluded from this calculation.
High perfect use effectiveness rates, ones that approach 100%, demonstrate that a treatment works, as long as participants follow all of the instructions correctly.
The Typical Use Effectiveness Rate
To calculate the typical use effectiveness rate, the researchers take the same study and crunch the numbers differently. The typical use rate is the percentage of people who achieved the desired outcome, regardless of whether or not they followed the regimen correctly. For this calculation, everyone who participated in the study is included, including those who didn’t follow the treatment instructions. The typical use rate does not discriminate. Regardless of the reason the participant didn’t follow the instructions – whether they were not motivated, they didn’t fully understand the instructions, or the instructions were too hard to follow, they will still be included in the typical use rate of the study.
To illustrate: A study that results in a perfect use effectiveness rate of 95% and a typical use effectiveness rate of 90% means:
- 95% of the study participants achieved the desired outcome while following all the directions perfectly (and 5% of the study participants didn’t experience the desired outcome, even though they followed the directions perfectly).
- 90% of the study participants were successful overall, including those that strayed from the instructions. So, at the end of the study, 90% of the people who enrolled in the study achieved the desired outcome. This number is the total success rate of the study.
You might be thinking (especially if you’re thinking ahead to NFP) that you can dismiss the significance of typical use effectiveness rates. What’s the point of tracking all the people who didn’t follow the instructions? Isn’t medical research about finding out what works, biologically? Well, yes and no.
The secret to understanding perfect use and typical use effectiveness rates is to know that they are meant to be compared. Considering one without the other gives an incomplete picture of a treatment’s effectiveness. We can learn a lot about medical treatments by comparing the perfect and typical use rates.
A Silly Example
Imagine a treatment for chronic pain that requires you to:
- Take a pill every two hours during the day and every four hours at night.
- The pill must be taken with 125 mL of lukewarm water.
- The pill must be taken while standing on one foot.
What might a study on the effectiveness rates for this treatment reveal? Assuming that the medication itself was highly effective, the perfect use effectiveness rate for this study might well be nearly 100%. The study participants that did everything right, all the time, experienced complete relief of their pain. Hurrah!
However, how many people fell into the “typical use” category? And how did it turn out for them? It’s likely that a lot of study participants would find it difficult to follow these instructions perfectly.
- There’s going to be some people who forget to take a dose (or two) of their medication at some point through the day.
- Some people won’t have a cup that measures in milliliters, so they just drink with an unmeasured cup of water and think to themselves “that’s about half a cup—good enough!”
- Perhaps the doctor didn’t emphasize the importance of lukewarm water, and the participant takes the pill with cool water.
- Some other participants might have balked at the whole “on one foot” part and, perhaps a little rebelliously, swallowed their pills with two feet firmly planted on the floor.
There are potentially more serious reasons why some study participants might have deviated from the instructions, too.
- Some participants may have had an additional temporary ailment (like a sore throat) that was so painful they couldn’t swallow the pill.
- Some elderly participants might have had balance issues. Knowing that standing on one foot in the middle of the night would put them at risk for a fall, they took their nighttime pills sitting up in bed.
The typical use effectiveness rate reveals how real people fared. It shows how closely real people, in real life situations, were willing and able to follow the instructions.
Imagine that the perfect use rate for this study was 100%, but the typical use effectiveness rate was 72%. That difference would be significant … and one logical explanation for it would be that a significant percentage of the people in the study either couldn’t or didn’t want to follow the instructions precisely. Quite often, following the instructions precisely turns out to be a significant predictor of success! Maybe it actually was quite important that you took each pill while balancing on one foot!
So now that you know what the different types of effectiveness rates mean and why they matter, this is what you’re looking for when choosing an effective treatment:
- Ideally, the perfect use rate should be pretty close to 100%. This means that the treatment works. If you follow the instructions perfectly, you are very likely to experience the desired outcome.
- The typical use rate should be relatively close to the perfect use rate. The smaller the gap between the perfect use rate and the typical use rate, the better. This means that most of participants in the study achieved the desired outcome, even in real world conditions.
- A large discrepancy between the perfect use and typical use rates for a medical treatment would be a bit of a red flag. What it suggests is that a significant portion of the study participants found it difficult to follow the instructions perfectly, and that in that struggle, they weren’t able to experience the therapeutic effects of the treatment.
A wide gap between perfect and typical use rates doesn’t reveal why participants didn’t follow the instructions (Did they misunderstand the instructions? Were they insufficiently motivated, perhaps because—to take our silly example—their pain just wasn’t that bad? Were the instructions too complicated for some of the participants to remember?) Whatever the root cause, a wide gap between the perfect use and typical use rates for a medical treatment should give you pause, because it suggests that many people (and maybe people like you) found it difficult to follow the instructions perfectly, and as a result didn’t achieve the desired outcome.
Natural Family Planning Effectiveness Studies
Now let’s map these concepts onto natural family planning.
NFP effectiveness studies are, in some ways, simpler—at least numerically—than those for other medical treatments. The participants in the study either become pregnant, or they don’t—there isn’t much of a grey area. Unlike other medical treatments, defining success is simple—if couples were able to successfully avoid pregnancy over the span of the 1-year study, then the method was effective.
To set up an NFP method effectiveness study, researchers enroll a group of sexually active women who indicate they want to avoid pregnancy (these are women who are “trying to avoid” or TTA). The women will need to fit the specific criteria of the study—if it’s a study on women in regular cycles, then women who just had a baby and women who are approaching menopause won’t be included. The researchers teach the women how to practice the method correctly, including how to identify which days are fertile and which days are not. They direct women to abstain from intercourse on fertile days. A normal part of most modern NFP methods is “charting,” so, just like normal NFP users do, the women in the study keep a chart of their daily fertile signs and acts of intercourse.
At the end of the year, the researchers review the data to determine the success rate of the study. This is when the effectiveness rates will be calculated. The study will report the perfect use rate (sometimes called the correct use rate) and typical use rate (sometimes called the total pregnancy rate).
The perfect use effectiveness rate for a family planning method reflects the percentage of women in an effectiveness study who, over the course of one year, followed the method instructions perfectly and did not become pregnant. (It is important to point out that a 99% perfect use effectiveness rate does not mean a 1% chance of becoming pregnant each time you have intercourse. It’s a 1% chance of becoming unintentionally pregnant over the span of 1 year of using the method.)
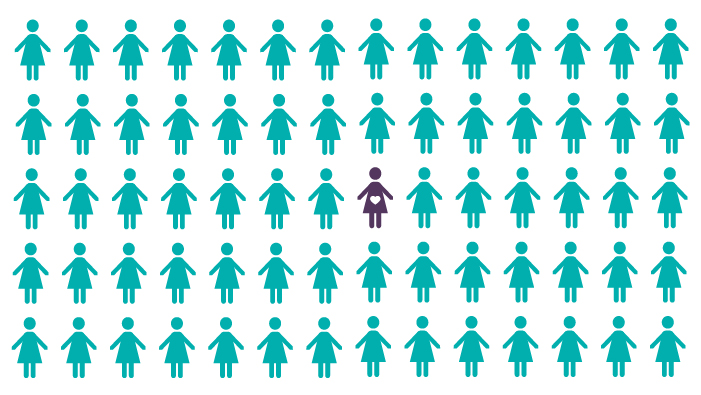
A perfect use effectiveness rate of 99% means that 1 woman out of 100 women over the course of one year experienced an unintended pregnancy, even though she followed the instructions correctly. That looks like this:

The typical use effectiveness rate reflects the total number of women who became pregnant over the course of the study. This number includes all the pregnancies in the study, including those that were the result of a couple either intentionally or unintentionally straying from the method instructions.
A typical use effectiveness rate of 95% means that 5 women out of 100 over the course of one year became pregnant, even though they checked off “avoid pregnancy” as their intention for the cycle in which they conceived. That looks like this:

The typical use effectiveness rate includes couples who became pregnant because they “took a risk” and engaged in intercourse on a day they knew to be potentially fertile. It also includes couples who became pregnant when they didn’t follow the method’s instructions for fertile observations 100% of the time, or who didn’t update their chart 100% of the time. In short, the typical use effectiveness rate is a “real-world” calculation that reveals how people fared when life happened.
To Sum up:
When you’re picking a method of pregnancy avoidance, look up and compare the perfect use and the typical use effectiveness rates. These two rates are meant to be compared and can tell you a lot about the method and help you to predict your likelihood of success.
While you’re digging into the research, here’s three more things to keep in mind:
1. Sample Size Matters
The larger the number of participants in the study, the better the results. If an effectiveness study only followed 4 participants, and 2 of them didn’t follow the instructions correctly and became pregnant, the perfect use rate would be 100% and the typical use rate would be 50%. Sure, that’s a wide discrepancy … but how representative were those couples? The larger the study, the more accurate the effectiveness rates (Peragallo Urrutia et al., 2018).
2. Location, Location, Location
Check to see where the study was located. How closely do you think the participant’s life situations resemble your life situation? Even though human bodies work the same the world over, there are perhaps surprising regional differences in NFP studies conducted in different countries. Here’s an anecdotal example: My Canadian clients tend to have a return to fertility while breastfeeding that’s significantly later than my American clients. Why? It’s hard to say. Perhaps it’s related to Canada’s maternity leave policies. Canadian women are entitled to 12-18 months of partially compensated maternity leave, and so many Canadian women don’t return to work until after their baby’s first birthday. Research shows that intensive breastfeeding delays a woman’s return to fertility, and a large percentage of Canadian women continue to breastfeed their babies during their year-long maternity leave. Location matters. In fact, NFP researchers have identified a need for more US-based effectiveness studies (Manhart & Fehring, 2018, p. 341).
3. Don’t be Confused by Different Terminology
Medical research is a little complex and can get a little jargon-y. The terms I’m using here—perfect use rate/correct use rate and typical use rate/total pregnancy rate—mean something quite precise. Something called “doctor error” or even “user error” (even if it’s expressed as a percentage) doesn’t necessarily mean the same thing as a typical use effectiveness rate calculated at the end of an effectiveness study. When in doubt, ask!
You’re now well prepared to dive into the research! As a nurse and Marquette Method Instructor, I’m all about informed consent. I want my clients to choose their method of NFP after weighing all their options and making the best choice for themselves and their family. I know that as couples weigh their options, they may decide to use a different method of NFP—they might not choose Marquette. That’s OK! There is no one NFP method that’s a perfect fit for all of humanity!
I really encourage you to look into the effectiveness rates of the modern methods of NFP. You can even compare the NFP effectiveness rates to the effectiveness rates of contraceptive options, which are measured and reported in the same way. You can find links to the Marquette Method’s regular cycles and postpartum effectiveness studies here (they are free and open access), as well as a link to a recent “State of the Field” review paper that provides the perfect and typical use effectiveness rates for many other modern methods of NFP.
Want to know how this all applies to the Marquette Method? Read the next article in this series, “How Effective is the Marquette Method of NFP?” where I provide a plain-language explanation of Marquette’s effectiveness research for women in regular cycles.
References: